How do full dental implants work? Full dental implants are an innovative solution to the age-old problem of tooth loss, offering a permanent and aesthetically pleasing option for those seeking restoration of their smile. The foundation of this groundbreaking procedure is based on mimicking natural tooth anatomy by surgically embedding titanium posts into the jawbone. This process serves as artificial tooth roots that bond with the bone in a remarkable healing phenomenon known as osseointegration. As a result, full dental implants not only restore appearance but also enhance functionality, allowing individuals to chew, speak, and engage in social interactions without the limitations often associated with traditional dentures or bridges. In this extensive guide, we will explore how dental implants function, the procedure involved, and the essential elements contributing to their success.
The need for full dental implants
To fully appreciate the transformative power of full dental implants, it’s crucial to understand the various reasons why individuals may find themselves needing them. Tooth loss can significantly affect one’s quality of life, and understanding its causes provides insight into the importance of restorative dentistry.
Common causes of tooth loss
Tooth loss can occur due to multiple factors, each leading to a decline in oral health and overall well-being.
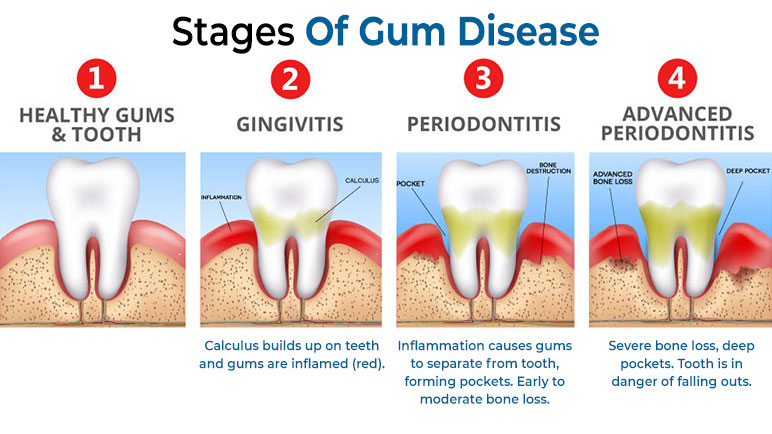
- Gum Disease (Periodontitis): One of the primary contributors to tooth loss is gum disease, which results from inflammation and infection of the gums. Over time, untreated gum disease destroys supporting tissues and bone around teeth, leading to mobility and eventual loss. Regular dental check-ups and proper oral hygiene can mitigate the risk, but awareness of symptoms is vital.
- Dental Caries (tooth decay): Another prevalent cause stems from dental caries or tooth decay, where bacteria produce acids that erode tooth enamel. If left untreated, cavities can progress to the point of requiring extraction. Prevention through good oral hygiene practices, fluoride treatments, and regular dental visits can reduce the occurrence of decay.
- Trauma or Injury: Accidents, whether they occur during sports or everyday activities, can lead to fractured or displaced teeth. Depending on the severity of the damage, extraction may be necessary. Awareness of safety measures and protective gear can help minimize the risk of injury leading to tooth loss.
- Genetic Predisposition: Some individuals carry a genetic predisposition to developing conditions that may increase their risk of tooth loss, such as weakened enamel or susceptibility to gum disease. Such predispositions highlight the importance of tailored dental care and preventive strategies.
- Systemic Diseases: Certain medical conditions like diabetes or autoimmune disorders can adversely affect oral health, making individuals more susceptible to infections and complications. Patients with these conditions should communicate openly with their dentists about their health history to ensure comprehensive dental care.
Impact of missing teeth on quality of life
The absence of teeth can have far-reaching implications on an individual’s quality of life, extending beyond mere aesthetics.
- Appearance and Confidence: The visual impact of missing teeth can be significant, altering one’s facial structure and leading to feelings of self-consciousness. Individuals often shy away from social situations due to embarrassment, perpetuating a cycle of diminished self-esteem.
- Speech and Pronunciation: Missing teeth can interfere with clear speech, creating communication barriers that frustrate both the speaker and listener. Teeth play a vital role in articulating certain sounds, and their absence can distort pronunciation, affecting relationships and professional opportunities.
- Chewing and Digestion: The inability to effectively chew food can lead to digestive problems. When teeth are missing, individuals may resort to softer foods that lack essential nutrients, ultimately resulting in nutritional deficiencies that compromise overall health.
- Oral Health: The loss of teeth can negatively impact the alignment and stability of remaining teeth, setting the stage for further loss and complicating future dental procedures. Moreover, the underlying jawbone may deteriorate without stimulation from the roots of healthy teeth, leading to additional issues.
- Social Interactions: The discomfort of speaking or smiling in public settings can hinder social interactions, isolating individuals from meaningful connections. By restoring function and aesthetics, full dental implants can reinstate confidence and facilitate engagement in diverse social situations.
Advantages of choosing full dental implants
Full dental implants present various advantages over alternative tooth replacement options, rendering them an appealing choice for many individuals facing tooth loss.
- Improved Aesthetics: One of the most significant benefits is the restoration of a natural-looking smile. Full dental implants seamlessly blend with surrounding teeth, providing confidence in one’s appearance.
- Enhanced Function: Implants function just like natural teeth, allowing individuals to enjoy their favorite foods without restrictions. With stable support, chewing and speaking become much more comfortable.
- Preservation of Jawbone: Unlike traditional dentures, full dental implants stimulate bone growth, preventing the deterioration that typically follows tooth loss. This preservation contributes to maintaining facial structure and overall oral health.
- Durability and Longevity: With proper care, full dental implants can last a lifetime. Their robust materials and construction provide a long-term solution, reducing the need for frequent replacements associated with other options.
- Improved Oral Health: Full dental implants require no alterations to adjacent teeth, preserving the integrity of natural tooth structures. This approach prevents further dental issues down the line, ensuring better oral and overall health.
- Increased Comfort and Confidence: The stability and realistic feel of implants provide enhanced comfort and boost confidence during social interactions, allowing individuals to smile widely without fear of embarrassment.
How full dental implants work
To comprehend how full dental implants work, we must delve deeper into the specific processes and components that contribute to their effectiveness.
Overview of the implant procedure
The journey toward achieving full dental implants begins with a detailed assessment and careful planning. The procedure involves placing titanium posts into the jawbone, serving as artificial roots for prosthetic teeth. These implants fuse with the bone over time, creating a stable foundation to support the final restoration.
During the implant procedure, patients undergo various stages, including pre-implant assessments, surgical placement of the implants, healing periods for osseointegration, and finally, the attachment of customized prosthetic restorations. Each step is paramount to ensure optimal results.
Components of a full dental implants
Understanding the individual components of a full dental implant system is integral to grasping how they function.
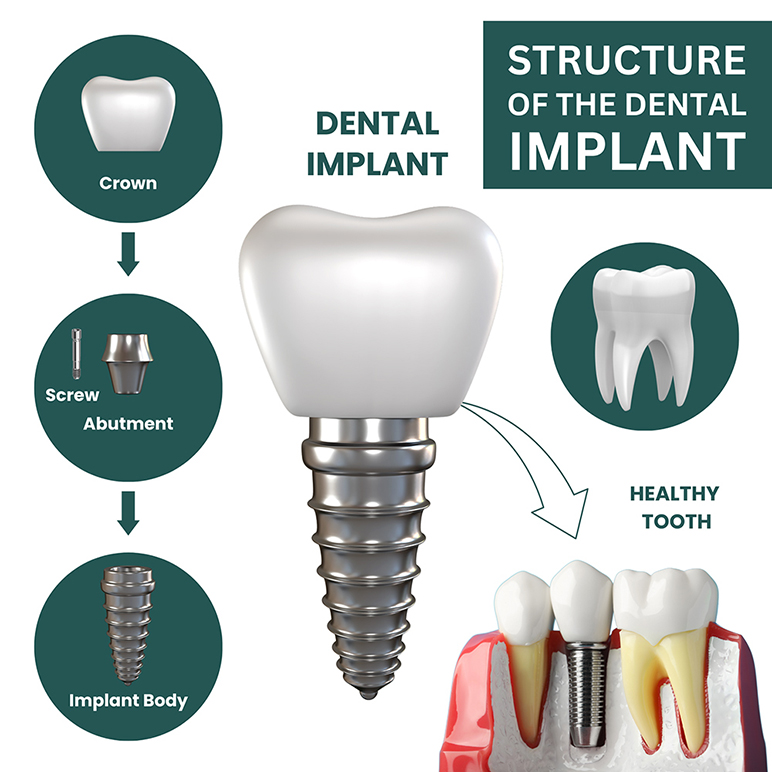
- Implant Fixture: At the core of a dental implant is the titanium post, known as the implant fixture. This durable material is biocompatible, allowing it to bond with the surrounding bone effectively. The implant fixture acts as the artificial root, anchoring the entire restoration securely.
- Abutment: Attached to the implant fixture is the abutment, a connector piece that links the implant to the visible prosthetic restoration. Abutments come in various shapes and sizes, tailored to accommodate different types of restorations, whether crowns, bridges, or full dentures.
- Restoration: The visible part of the implant system is the restoration, designed to resemble natural teeth closely. Depending on an individual’s needs, the restoration may consist of a single crown, a bridge that spans several missing teeth, or a full denture that replaces an entire arch.
The healing process and osseointegration
A critical aspect of how full dental implants work lies in the healing process, particularly osseointegration—the biological bonding of the implant with the jawbone.
Osseointegration is facilitated by the inherent properties of titanium, which allow it to integrate seamlessly with bone tissue. During the healing period following implant placement, which can last several months, the body works to form new bone cells around the implant fixture, stabilizing it within the jaw.
The success of osseointegration hinges on several factors, including the patient’s overall health, bone density, meticulous adherence to post-operative care instructions, and lifestyle habits. Patients must follow guidelines to promote healing, such as avoiding strenuous activity and adhering to prescribed medications.
Pre-implant assessment and planning
Before embarking on the journey toward full dental implants, thorough assessment and planning are essential to achieve optimal outcomes.
Importance of comprehensive dental evaluation
A comprehensive dental evaluation sets the stage for successful implant placement. This assessment helps identify potential challenges and tailor the treatment plan accordingly.
- Assess Bone Density and Quality: Adequate bone density is crucial for successful implant placement and osseointegration. Dentists utilize X-rays and 3D imaging techniques to determine if sufficient bone exists or if supplementary bone grafting is required.
- Evaluate Oral Health: Understanding a patient’s oral health status—such as the presence of gum disease or infections—is paramount before implant placement. Any existing conditions must be addressed to ensure a strong foundation for implants.
- Review Medical History: A patient’s medical history plays a critical role in treatment planning. Patients with systemic diseases, such as diabetes or bleeding disorders, may require specific adjustments to the treatment plan to mitigate risks.
- Determine Suitability for Implants: The dentist evaluates the patient’s anatomy, jaw structure, and overall health to assess candidacy for dental implants. Factors like lifestyle, habits, and expectations are also considered to develop a personalized approach.

Diagnostic imaging techniques
Technology has revolutionized the diagnostic process, enhancing the accuracy of assessments conducted prior to implant placement.
- Panoramic X-rays: These provide a comprehensive view of the upper and lower jaws, allowing dentists to assess the size, shape, and positioning of existing teeth and supporting bone structures. Panoramic imaging provides valuable information for strategic planning.
- Cone Beam Computed Tomography (CBCT): This advanced 3D imaging technique generates detailed images of the jawbone, revealing critical information about bone density, nerve pathways, and anatomical structures pertinent to implant placement. CBCT scans play a pivotal role in accurately mapping the surgical site.
- Digital Impressions: Utilizing digital scanners, dentists can create precise virtual models of the mouth and teeth. These impressions facilitate the design and fabrication of custom-made dental restorations, ensuring optimal fit and aesthetics.
Custom treatment plans
Based on the pre-implant assessment, the dentist crafts a personalized treatment plan tailored to meet the specific needs and goals of the patient.
- Number and Location of Implants: The treatment plan specifies the optimal number and placement of implants required to support the desired restoration. Strategic placement ensures stability and balance within the oral cavity.
- Type of Restoration: Based on patient preferences, the dentist recommends the most suitable prosthetic restoration, whether it be a full denture, fixed bridge, or another option. The choice largely depends on the extent of tooth loss and individual needs.
- Bone Grafting (if needed): Should the jawbone lack sufficient density to support implants, a bone graft procedure may become necessary. Bone grafting augments the bone, providing a solid foundation for implant placement and improving overall outcomes.
- Timeline and Stages of Treatment: The treatment plan outlines the various stages involved in the implant procedure, including surgery, the healing period, and restoration placement. This timeline assists patients in understanding what to expect throughout the process.
The implantation process
Once the pre-implant phase is complete, patients move forward to the implantation process, where the actual procedure takes place.
Anesthesia and sedation options
The comfort of the patient is paramount during implant placement, and various anesthesia and sedation options exist to accommodate differing levels of anxiety and complexity.
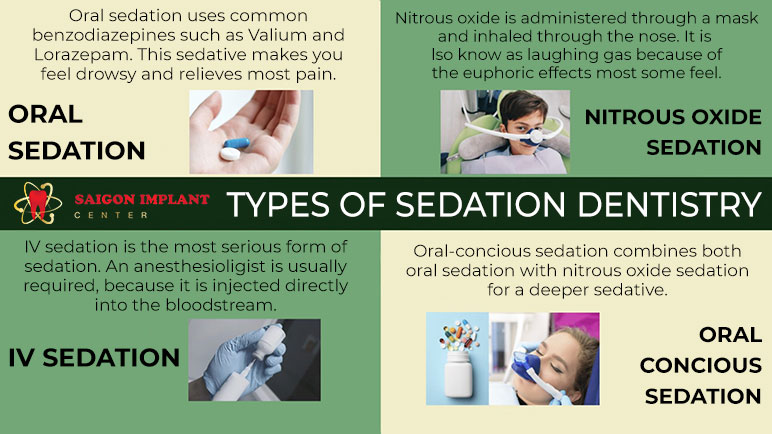
- Local Anesthesia: The most common choice is local anesthesia, numbing the area surrounding the implant site, allowing the procedure to proceed with minimal discomfort.
- IV Sedation: For patients who experience anxiety or require more extensive procedures, IV sedation can be administered. It induces a relaxed state, helping patients remain calm and comfortable during the operation.
- General Anesthesia: In cases involving complex scenarios or patients with severe dental anxiety, general anesthesia may be utilized. This deeper level of sedation renders the patient unconscious throughout the procedure, alleviating any discomfort or stress.
Step-by-step surgical procedure
The surgical process itself comprises several critical steps, ensuring the safe and effective placement of the dental implants.
- Incision and Flap Creation: The first step involves making a small incision in the gum tissue, exposing the underlying jawbone. Precision is key, as the surgeon seeks to minimize trauma to surrounding tissues.
- Pilot Hole Drilling: Specialized drills are employed to create small pilot holes in the jawbone, preparing it for the implant fixture. Accurate drilling is essential to ensure that the implant is placed at the correct angle and depth.
- Implant Fixture Placement: The titanium implant fixture is carefully inserted into the prepared hole in the jawbone, establishing a secure anchor for the restoration.
- Closure of the Incision: Once the implant is in place, the gum tissue is stitched closed around the fixture. This closure allows for optimal healing while protecting the surgical site from external factors.
- Healing and Osseointegration: Following the placement, the implant requires time to fuse with the bone—a process that typically takes several months. Adequate healing is essential for long-term success.
- Abutment Placement: Once osseointegration is confirmed, a small connector piece called the abutment is attached to the implant fixture. This serves as a link between the implant and the final restoration.
- Impression Taking and Restoration Fabrication: A dental impression is taken to create a precise model of the mouth, enabling the fabrication of a custom-made prosthetic restoration in a dental laboratory.
- Restoration Placement: The final prosthetic restoration is securely attached to the abutment, completing the implant procedure and restoring function and aesthetics.
Immediate post-operative care
Following the implant placement surgery, patients must adhere to specific post-operative care instructions to promote healing and minimize complications.
- Medication Management: Pain relievers and antibiotics may be prescribed to manage discomfort and prevent infections. Adhering to the medication regimen is crucial.
- Oral Hygiene: Maintaining meticulous oral hygiene is vital, even after surgery. Patients should use a soft-bristled brush and gentle rinsing techniques to keep the area clean without disturbing the surgical site.
- Dietary Restrictions: Following a soft food diet for the initial healing period is recommended to avoid stressing the surgical site. Foods that are easy to chew and digest will aid in recovery.
- Avoiding Smoking and Alcohol: Smoking and alcohol consumption can impede healing and increase the risk of complications. Patients are encouraged to abstain from these substances during the recovery period for the best outcome.
Maintenance and longevity of full dental implants
Ensuring the longevity of full dental implants requires commitment and diligent maintenance. A proactive approach to oral health can greatly influence the lifespan of implants.
Daily oral hygiene practices
Maintaining excellent oral hygiene practices is fundamental to the longevity of dental implants.
- Brushing and Flossing: Patients should brush their teeth at least twice daily and floss regularly to remove plaque and food particles. Special attention should be paid to the implant and abutment areas to prevent peri-implantitis.
- Use of Antimicrobial Rinses: Incorporating antimicrobial mouth rinses can help control oral bacteria and reduce the risk of infection around the implant site. Always consult with a dentist to choose appropriate products.
- Regular Check-Ups: Routine dental visits for professional cleanings and evaluations are vital in monitoring the condition of dental implants. Dentists can identify potential issues early on, preventing complications before they arise.

Regular dental check-ups
Patients with full dental implants should prioritize regular dental check-ups to ensure ongoing health and monitoring of the restorations.
- Comprehensive Evaluations: During check-ups, dentists assess the condition of the implants, surrounding gum tissue, and overall oral health. Identifying signs of infection or complications early can lead to timely intervention.
- Professional Cleanings: Regular professional cleanings not only promote oral hygiene but also assist in detecting any concerns related to the implants. Cleaning around implants requires specialized techniques to preserve their integrity.
- Radiographic Assessments: Periodic X-rays enable dentists to observe changes in the bone surrounding the implants. Ongoing evaluation helps maintain the health of both implants and jawbone.
Factors affecting implant longevity
Several factors determine the longevity of dental implants, ranging from patient habits to overall health.
- Patient Compliance: Adhering to oral hygiene routines and attending scheduled dental appointments significantly affects the success of dental implants. Patients must actively participate in maintaining their dental health.
- Lifestyle Choices: Habits such as smoking and excessive alcohol consumption can jeopardize the success of dental implants. Individuals are strongly advised to adopt healthier lifestyles that promote healing and oral health.
- Underlying Health Conditions: Systemic health issues can influence the outcomes of dental implant procedures. Conditions such as uncontrolled diabetes or autoimmune disorders may pose risks. Therefore, open communication with healthcare providers is essential.
Conclusion
Full dental implants represent a revolutionary solution for individuals struggling with tooth loss, combining aesthetics, functionality, and durability. Understanding how they work, the intricacies of the implantation process, pre-implant assessments, and ongoing maintenance requirements highlights the significance of informed decision-making when considering this treatment option. Through advancements in technology and techniques, dental professionals can offer patients personalized solutions that restore not only smiles but also confidence and quality of life. As we continue to embrace dental innovations, the path to achieving functional and beautiful smiles remains bright, empowering individuals to regain control over their oral health and overall well-being.

 Google Reviews
Google Reviews Call
Call
SAIGON IMPLANT CENTER
Best dentist in Vietnam
Saigon Implant Center - Dental Clinic utilizes the latest technology for specialized treatment in the field of Single implant, full jaw implants, All on 4 implants, All on 6 implants, Zygoma implant....
SAIGON IMPLANT CENTER
Best dentist in Vietnam
Saigon Implant Center - Dental Clinic utilizes the latest technology for specialized treatment in the field of Single implant, full jaw implants, All on 4 implants, All on 6 implants, Zygoma implant....